In this modern age of mounting legislation, environmental concerns, occupant health and safety and increasing onus on cost-efficiency, a facility manager's responsibilities and considerations are growing in complexity. Take the washroom, for example. An FM’s principal concerns focus on hot water safety, water efficiency and hygiene, functionality and maintenance. However, Legionella control is not always a foremost priority for some commercial premises.
Rising risk
To better understand the need to place sharpened focus on Legionella control measures and practices, FMs must first consider the scope of the risk.
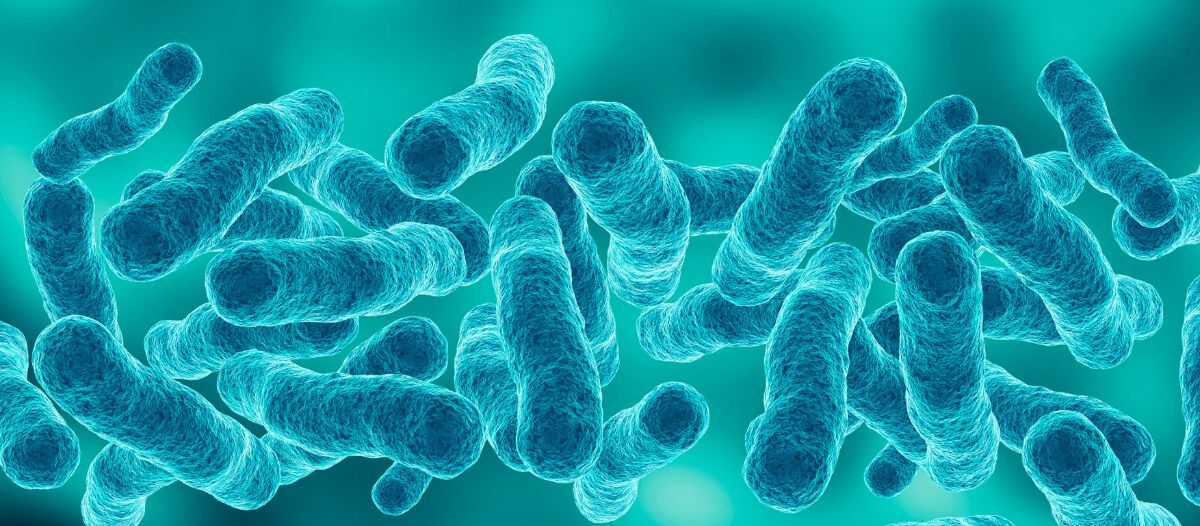
Legionella is a naturally occurring bacteria widespread in ponds, rivers and other natural water systems. When this bacterium enters water systems in the built environment, conditions such as water temperature and ineffective disinfection levels can encourage rapid growth. Common sources of Legionella bacteria in buildings include cooling towers, taps, showers, air conditioning units and hot water tanks.
Legionnaires’ disease is a potentially fatal lung infection caused by inhaling droplets of water containing Legionella bacteria. If the infection is not contained or treated early, it can cause confusion, coma, heart failure or death.
According to the World Health Organization (WHO), the death rate for Legionnaires’ disease in untreated immunosuppressed patients could be as high as 40-80 percent. Moreover, Legionnaires’ disease is known to cause health-related quality of life impacts to the large majority people who have recovered from it. These include fatigue, neurologic and neuromuscular symptoms and post-traumatic stress disorder.
 The Legionella risk is rising. In the U.S., the incidence of Legionellosis has surged by approximately 1,000 percent over the past two decades, with countless more global incidents going unreported or undiagnosed. Factors such as climate change, warming temperatures and increasingly complex water systems have all contributed to the rapidly increasing count.
The Legionella risk is rising. In the U.S., the incidence of Legionellosis has surged by approximately 1,000 percent over the past two decades, with countless more global incidents going unreported or undiagnosed. Factors such as climate change, warming temperatures and increasingly complex water systems have all contributed to the rapidly increasing count.
Importantly, the risk of Legionella proliferation is generally greater in commercial premises. Foremost, commercial properties often have larger and more intricate water systems, including cooling towers, air conditioning units and extensive plumbing networks, which provide more opportunities for Legionella bacteria to grow and spread. One study found that cooling towers in particular, commonly found in industrial and commercial businesses, have contamination rates as high as 49 percent in some regions.
Also, larger commercial buildings have more extensive water networks, increasing the potential for stagnant water and areas of low water flow, which are conducive to Legionella growth. The scope for periods of low occupancy or disuse brings further risk due to water stagnation, creating ideal conditions and breeding grounds for Legionella growth.
Best practice challenges
Of course, the established approach among FMs to prevent Legionella growth is simple: hot water should be stored above 60 C (140 F) and distributed above 50 C (122 F), while cold water storage and distribution should be below 20 C (68 F). Infrequently used outlets should be flushed regularly, and all outlets should be de-scaled and cleaned as required.
As part of this, thermostatic mixing valves (TMVs) are typically used to allow water to be stored and distributed at the required temperature to kill harmful Legionella bacteria; but reduced to a safe temperature at the point of use by mixing it with cold water supply.
However, while TMVs are essential for minimizing the risk of scalding, they can inadvertently increase the risk of Legionella growth. This is because the blended water downstream of a TMV can create an environment conducive to the bacteria's multiplication. Ensuring safe TMV use depends on implementing a robust maintenance program, including regular flushing to prevent water stagnation — a known factor for promoting Legionella. Despite this, the consensus is that TMV maintenance, inspections and servicing are not necessarily as thorough as they should be. The scope for periods of low occupancy or disuse leads to water stagnation and increased risk of bacterial growth.
The result is that it is becoming more important than ever for FMs to pay extra diligence to how they assess, test and control the risk of exposure to Legionella bacteria in the face of changing environmental conditions.Better detection, better protection
So, what is to be done? Foremost, the recommendation is for FMs to prioritize more frequent and more robust water quality testing for Legionella in distribution systems.
Most FMs are well acquainted with the standard lab-culture method, whereby water samples are collected from on-site water systems and sent to an accredited laboratory that will identify the presence or absence of Legionella. However, this approach is time-consuming, cumbersome and has limitations.
Most lab culture tests take 7-10 days to return results. Yet Legionella can double in a day. This lag time means increased exposure and risk for FMs and the premises they serve. Water samples can also get damaged in the transportation process, potentially killing the Legionella inside and increasing the risk of a false negative result. Lab culture testing is also unable to detect viable but nonculturable Legionella (VBNC) – which, though dormant, can still be incredibly dangerous due to their ability to resuscitate and reinfect a water system. It can also directly infect human cells while in their dormant state. The result can be a false sense of security, with the potential for lab results to state a negative outcome when repeated subsequent tests confirm nonconformance.
As Legionella risk evolves, there is a clear case for FMs to consider including rapid testing as part of the Legionella testing process.
Designed to overcome the limitations of traditional Legionella detection, the latest generation of rapid testing kits enable the detection of Legionella in just 25 minutes and are incredibly accurate at quickly detecting the most common and potentially fatal species of Legionella bacterium: Legionella pneumophila.
To confirm its accuracy, a study conducted by the CDC ELITE laboratory Chemicals Incorporated (CHEM Inc.), saw Legionella samples tested using both the traditional lab-culture testing and a rapid testing kit. The study revealed a rapid test solution is 100 percent accurate in identifying both Legionella pneumophila serogroup 1 and serogroups 2-15 from blind samples and gave comparable results to the traditional lab-culture testing method but in a much quicker time.
Detecting Legionella pneumophila quickly empowers FMs to react promptly to contamination and take appropriate action, thereby significantly minimizing the risk of exposure and human infection. Not only does using this method for routine testing help reduce risk and minimize potential exposure to building occupants, it also offers additional information during necessary reviews of the risk assessment.
Safety first
Legionnaires’ disease remains a serious and rising risk to the public, and as such, the correct management and control of Legionella has never been more critical.
As the frontline defenders against this potentially deadly bacterium, FMs are already responsible for implementing and overseeing comprehensive water management plans to include regular risk assessments and ensuring that all water systems are regularly inspected and maintained. By incorporating next-generation rapid Legionella testing technology into their safety protocols, FMs have an opportunity to ensure due diligence, minimize legal liabilities, safeguard the health of all individuals within their premises and – ultimately – raise the bar in promoting an absolute best practice approach when it comes to the prevention of diseases associated with Legionella.

Greg Rankin, CEO, Hydrosense, is a seasoned technology product veteran with a deep passion for protecting public health from Legionella bacteria. With a decades of experience in technology, marketing, and business development, Rankin's expertise spans end-to-end marketing and product management, with a strong focus on meeting customer’s needs. His career has seen him hold key roles at leading companies such as Oracle, Ingenico and Metaforic, as well as a number of startups, where he honed his skills in delivering innovative solutions to global markets. He fosters a culture of trust, values diversity, and encourages a 'test and learn' approach within his team. He is dedicated to raising awareness about the broader risks of Legionella outbreaks, advocating for greater vigilance and early detection in all sectors.
Read more on Risk Management or related topics Occupant Health and Risk Management
Explore All FMJ Topics